Connect With Us
Blog
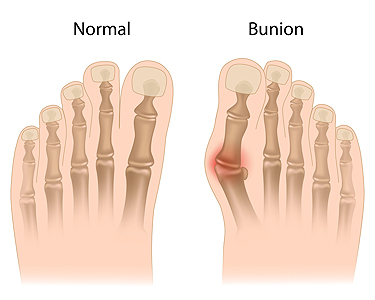
Bunions, a prevalent foot deformity, are characterized by a bony bump that forms at the base of the big toe. Contrary to common belief, bunions are not merely a cosmetic issue but can cause discomfort and affect mobility. One essential fact about bunions is their tendency to develop gradually over time, often due to structural issues in the foot, such as flat feet or abnormal bone alignment. Additionally, wearing ill-fitting shoes, particularly those with narrow toe boxes, can exacerbate bunion development or worsen existing symptoms. Individuals with bunions may experience pain, swelling, redness, and restricted movement in the affected toe. Despite popular misconceptions, bunions cannot be permanently corrected through nonsurgical means. However, conservative measures such as wearing supportive footwear, and using orthotic inserts can help alleviate symptoms and slow the progression of the deformity. For severe cases causing significant pain or hindering daily activities, surgical intervention may be necessary to realign the affected joint and provide lasting relief from bunions. If you have a bunion, it is suggested that you are under the care of a podiatrist who can help you to manage this condition.
If you are suffering from bunions, contact Dr. Richard Silverstein of Union Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Preventing falls in the workplace is essential in ensuring the safety and well-being of employees. Falls can occur in any work environment, from construction sites to office buildings, and can result in serious injuries or even fatalities. Implementing proactive measures to mitigate fall risks is vital. This includes maintaining clean and clutter-free walkways, promptly addressing spills or slippery surfaces, and ensuring proper lighting in all areas of the workplace. Employers should also provide appropriate training on fall prevention techniques and the proper use of safety equipment such as harnesses, guardrails, and non-slip footwear. Regular inspections of equipment and work areas can help identify and address potential hazards before accidents occur. Encouraging open communication between management and employees regarding safety concerns fosters a culture of awareness and accountability. Falling can impact the feet, and may compromise completing daily activities. If you have injured one or both feet during your workday, it is suggested that you consult a podiatrist who can treat any foot condition you may have endured.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Dr. Richard Silverstein from Union Foot Care. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Selecting the appropriate footwear is important for medical employees, whose demanding roles require long hours of standing, walking, and patient care. The right shoes not only enhance comfort and alleviate fatigue but also play a critical role in preventing foot problems and injuries. Medical professionals often face unique challenges, such as exposure to bodily fluids, slippery surfaces, and the need for sterile environments. Therefore, shoes with non-slip soles, waterproof materials, and easy-to-clean surfaces are essential to ensure safety and hygiene. Additionally, supportive footwear with adequate cushioning, arch support, and shock absorption helps reduce strain on the feet, ankles, and lower back, minimizing the risk of musculoskeletal issues and promoting overall well-being. By investing in quality shoes that cater to their specific needs, medical employees can maintain optimal performance and focus on patient care. If you have foot pain from wearing shoes that do not fit well during your work day, it is suggested that you contact a podiatrist who can offer help to remedy your discomfort.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact Dr. Richard Silverstein from Union Foot Care. Our doctor will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016