Connect With Us

How to Get a Proper Shoe Fit
Many people suffer from foot problems because their shoes are poorly fitted. When shopping for a new pair of shoes, fashion usually triumphs over comfortability. A pair of well fitted shoes is essential in preventing foot problems and potential injuries.
Poorly fitted shoes can cause foot issues such as plantar fasciitis, bunions, hammertoes, ingrown toenails, and foot pain. Shoes such as high heels and sandals may cause problems for your feet. These shoes put the foot in an unnatural position for long periods and fail to provide good foot support. It is recommended to not wear either one for an extended period.
When you are trying on shoes, make sure they have enough space for your toes to move around. Shoes shouldn’t be cramped but also shouldn’t have too much room that your foot moves around in them. A snug shoe is a good choice. They should also provide good arch support and cushioning. Athletic shoes tend to offer both good support and cushioning. A degree of flexibility is necessary so they aren’t too stiff or too unsupportive.
If you can wear your shoes for a long period of time without experiencing any discomfort, this is a sign that your shoes fit properly. Do not be too dismayed if the shoe isn’t a perfect fit at first; many shoes take a few days to weeks to properly break in. However don’t expect an uncomfortable shoe to become fitted to your foot.
For those with foot conditions such as flat feet or pronation, orthotics may be helpful or even necessary to prevent foot pain. Orthotics are inserts that are placed in the shoe and provide support and cushioning for the foot. While there are many types of orthotics out there, custom-made orthotics may be necessary depending upon your foot and foot conditions.
Feet change in size over time. It is important to check your foot size over time so that you can make sure you have the perfect fit for your feet. A podiatrist can provide more information on proper shoe fitting and foot orthotics.
Ways Seniors Can Maximize Foot Care
 As one ages, it becomes harder to reach down to the toes and keep toenails trimmed properly. In some cases, just gripping the clippers is difficult, if not impossible. At the same time, toenail growth decreases with age, resulting in thicker nails that are more difficult to trim. One way to soften the thicker nails and make them easier to cut is by soaking the feet for about 10 minutes in warm water. Thoroughly dry the feet, and use a clipper to make small cuts straight across the nail to lessen the chance of an ingrown toenail. If your toenails have both hardened and become discolored, you may also have developed a fungal infection. Such a condition can worsen rapidly and become painful. For that reason, it would be wise to contact a podiatrist immediately, as fungal infections may take months to eliminate. It is also suggested that seniors make regular appointments with a podiatrist for proper foot-care treatment as needed.
As one ages, it becomes harder to reach down to the toes and keep toenails trimmed properly. In some cases, just gripping the clippers is difficult, if not impossible. At the same time, toenail growth decreases with age, resulting in thicker nails that are more difficult to trim. One way to soften the thicker nails and make them easier to cut is by soaking the feet for about 10 minutes in warm water. Thoroughly dry the feet, and use a clipper to make small cuts straight across the nail to lessen the chance of an ingrown toenail. If your toenails have both hardened and become discolored, you may also have developed a fungal infection. Such a condition can worsen rapidly and become painful. For that reason, it would be wise to contact a podiatrist immediately, as fungal infections may take months to eliminate. It is also suggested that seniors make regular appointments with a podiatrist for proper foot-care treatment as needed.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Dr. Richard Silverstein from Union Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Elderly and their Feet
While proper foot care is important for everybody, senior citizens have the tendency to be more susceptible to certain foot conditions. The elderly should therefore be well informed about any problems that may arise and about what they can do to properly avoid or treat them.
Some of the most common foot problems seniors are susceptible to include foot ulcers, ingrown toenails, fallen arches, and fungal nails. A foot ulcer is an open sore on the foot and can be a result of diabetes and decreased sensation in the feet. An ingrown toenail is defined as when the nail grows into the side of the toe. Fallen arches are indicated by the instep of the foot collapsing. A fungal nails is a condition that results in deformed and discolored toenails.
In order to avoid these conditions it is recommended that the feet be inspected by the patient on a regular basis. If these inspections are carried out routinely, there is a good likelihood that problems can be identified before they become severe, or can even be avoided altogether. If any abnormality is discovered, it is important that the individual consult a podiatrist for diagnosis and information on treatment options.
Proper foot hygiene is also important. Making sure that you always have clean, dry socks on can be a major deterrent to many different problems including bacterial infections, foot odor, and certain types of fungus. Wet feet are a major cause of many of these problems. If your socks get wet, it is important to change them. Walking around in wet socks may not only lead to various infections, but can irritate the skin and result in a number of various complications. Clean, dry feet are less likely to be affected by fungal and other infections.
As people age, the fat present on your feet begins to deteriorate. The protective nature of this fat keeps the feet healthy by providing a barrier between your bones and the ground. This also aids in giving the skin on the feet a certain amount of elasticity. This is one factor that causes elderly people to develop some serious foot issues. Foot moisturizers can be helpful to avoid certain problems associated with this. However, water-based moisturizers do not work as well for elderly people as they do for the young. Instead, it is more effective to use an emollient instead. An emollient is effective because it binds the water in the foot, keeping it from becoming absorbed too readily which will result in dry skin. Emollients also have a special property called occlusion, which provides a layer of oil on the skin. This layer prevents the foot from drying up and can be very effective in treating dry skin disorders. If you can keep the skin on your feet healthy, this will substantially reduce the number of foot problems you will encounter in old age.
Proper footwear is another way to keep feet healthy. Shoes that fit well and provide proper support help prevent ingrown toenails and fallen arches.
Certain medical conditions such as diabetes or poor blood circulation increase the risk for foot issues. For individuals with any of these conditions it is extremely important to conduct regular foot inspections to make sure that there are no sores or infections present.
Sports Related Foot And Ankle Injuries
Foot and ankle injuries are common among people who participate in sports. Several factors contribute to this. They include failing to stretch or warm up properly, not wearing the proper type of shoe and not taping or providing other types of support for the ankle or foot. The most common foot and ankle injuries suffered by people involved in sports are plantar fasciitis, ankle sprains and Achilles tendon damage or ruptures. If not treated properly, they can lead to permanent disability.
Treating these injuries is relatively simple if they are identified and addressed early. Many athletes dismiss the initial aches and pains associated with injury as just soreness or tired muscles. Their first response is usually to try to work through it. This can lead to serious problems. Many minor injuries are made far more serious when athletes continue to put strain and pressure on them. That attitude can change a mild strain into a serious strain and a minor tear into a rupture. Athletes should have unusual aches and pains evaluated by a skilled medical professional.
Plantar fasciitis is a painful injury. It is inflammation of the plantar fascia, the thick band of tissue running from the heel to the base of the toes. If left untreated, it can lead to a degenerative disease called plantar fasciosis. There are several effective treatments for this ailment. Doctors often prescribe rest, massages, stretching, night splints, physical therapy, anti-inflammatory medication, corticosteroids or surgery, usually in that order. The most effective treatment for plantar fasciitis is orthotics, which offers foot support. Surgery is occasionally used as a last resort, but it comes with the risk of nerve damage and infection and often does not stop the pain.
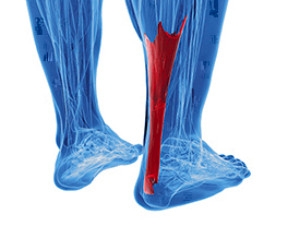
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone. Running, jumping and walking all impact this tendon. Two common injuries to the Achilles tendon are tendonitis and a rupture of the tendon. Tendonitis is inflammation in the tendon often caused by an increase in the amount of stress placed on it. Non-surgical treatments include rest, ice or anti-inflammatory medication. A rupture (tear) of the Achilles tendon can be treated by placing the lower leg in a cast for several weeks or with surgery. Many physicians feel surgery is the better option because it lowers the risk of re-ruptures. Both methods require 4 to 6 months of rehabilitation.
Ankle sprains are the most common sports related foot and ankle injury. A sprain occurs when the ligament holding the ankle bones and joint stretches beyond its normal range. It can be treated non-surgically with a combination of rest, ice wrapped around the joint for 30 minutes immediately after injury, compression by a bandage and elevating the ankle above the heart for 48 hours. This combination is referred to as RICE. Severe ankle sprains in which the ligaments are torn may require reconstructive surgery followed by rehabilitation.
Potential Achilles Tendon Injuries
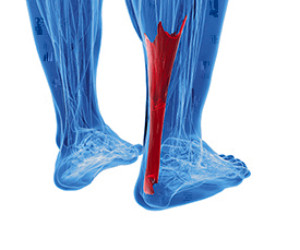 If you feel the back of your ankle, you will notice the fibrous tissue that connects the heel bone to the calf muscle. This is known as the Achilles tendon. There are two injuries that commonly affect this tendon. The first, known as Achilles tendinopathy, occurs when there is pain on the back of the heel as a result of overuse. Common signs of Achilles tendinopathy include swelling, stiffness, and pain that is worse in the morning. The second injury is an Achilles tendon rupture or tear, which commonly occurs as a result of jumping and pivoting with a lot of force. This causes the tendon to overstretch and eventually tear. Anyone who tears their Achilles tendon will notice a severe pain and a loss of both movement and strength in the tendon. If you are experiencing pain or swelling in your Achilles tendon, it is suggested that you consult with a podiatrist who can help provide a treatment option for injuries as well as ways to prevent a rupture.
If you feel the back of your ankle, you will notice the fibrous tissue that connects the heel bone to the calf muscle. This is known as the Achilles tendon. There are two injuries that commonly affect this tendon. The first, known as Achilles tendinopathy, occurs when there is pain on the back of the heel as a result of overuse. Common signs of Achilles tendinopathy include swelling, stiffness, and pain that is worse in the morning. The second injury is an Achilles tendon rupture or tear, which commonly occurs as a result of jumping and pivoting with a lot of force. This causes the tendon to overstretch and eventually tear. Anyone who tears their Achilles tendon will notice a severe pain and a loss of both movement and strength in the tendon. If you are experiencing pain or swelling in your Achilles tendon, it is suggested that you consult with a podiatrist who can help provide a treatment option for injuries as well as ways to prevent a rupture.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Richard Silverstein of Union Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
The 8 Principles of Foot Ulcer Prevention for Diabetics
The presence of diabetic peripheral neuropathy (nerve damage) and peripheral artery disease (poor circulation) in many diabetic patients creates a perfect storm of factors that can make wounds difficult to detect and take longer to heal. Chronic wounds that don’t heal (ulcers) are potentially very dangerous to both the overall health of the patient as well as their affected limb. There are eight steps every diabetic should take to help prevent such ulcers: 1) check your feet daily for cuts, growths or red spots, 2) wash and thoroughly dry your feet every day, 3) moisturize your feet, except between the toes, 4) trim your toenails straight across, but not too short, 5) avoid walking barefoot, and wear shoes that fit well, 6) protect your feet from extreme heat or cold, 7) elevate your feet as much as possible when sitting, and exercise your toes and ankles to aid circulation, and 8) have a podiatrist examine your feet at least once a year.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Richard Silverstein from Union Foot Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Solutions for Sweaty Feet
Do you regularly soak through your socks and shoes, regardless of the weather? Are you worried about leaving behind wet footprints when you walk around barefoot? Excessively sweaty feet may be a sign of a condition called plantar hyperhidrosis. In addition to being potentially embarrassing, this condition also increases your risk of various foot problems, such as fungal infections and injuries due to your feet slipping as you walk. Fortunately, various treatments are available for plantar hyperhidrosis. These include topical antiperspirants, iontophoresis, and botox injections into the foot. There are also special powders and shoe inserts that you can wear to absorb excess moisture. To learn more about treatments for plantar hyperhidrosis, and to find the right one for you, it’s suggested that you consult with a podiatrist.
If you are suffering from hyperhidrosis contact Dr. Richard Silverstein of Union Foot Care. Our doctor can provide the care you need to attend to all of your foot and ankle needs.
Hyperhidrosis of the Feet
Hyperhidrosis is a rare disorder that can cause people to have excessive sweating of their feet. This can usually occur all on its own without rigorous activity involved. People who suffer from hyperhidrosis may also experience sweaty palms.
Although it is said that sweating is a healthy process meant to cool down the body temperature and to maintain a proper internal temperature, hyperhidrosis may prove to be a huge hindrance on a person’s everyday life.
Plantar hyperhidrosis is considered to be the main form of hyperhidrosis. Secondary hyperhidrosis can refer to sweating that occurs in areas other than the feet or hands and armpits. Often this may be a sign of it being related to another medical condition such as menopause, hyperthyroidism and even Parkinson’s disease.
In order to alleviate this condition, it is important to see your doctor so that they may prescribe the necessary medications so that you can begin to live a normal life again. If this is left untreated, it is said that it will persist throughout an individual’s life.
A last resort approach would be surgery, but it is best to speak with your doctor to find out what may be the best treatment for you.
If you have any questions please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.