Connect With Us

Heel Pain and the Plantar Fasciitis
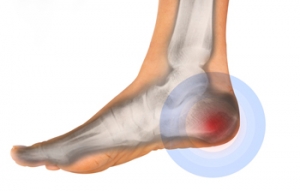
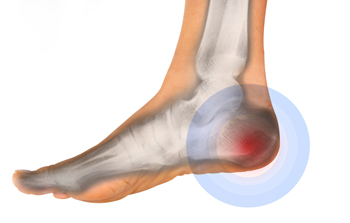 If you find you are experiencing heel pain throughout the day, especially in the morning, you may have a foot condition that is referred to as plantar fasciitis. Tenderness in the heel, a tingling sensation, or limping, are among the symptoms of plantar fasciitis. This condition develops as a result of the plantar fascia becoming torn, which may often be due to excessive strain the foot endures during physical activity. When this band of tissue that runs along the bottom of the foot becomes injured, patients will most likely feel intense heel pain. It’s important to have a proper diagnosis performed, and this may be accomplished by undergoing an MRI in addition to a physical examination. There are many treatment options available, and it’s suggested to schedule a consultation with a podiatrist who can choose the best one for you.
If you find you are experiencing heel pain throughout the day, especially in the morning, you may have a foot condition that is referred to as plantar fasciitis. Tenderness in the heel, a tingling sensation, or limping, are among the symptoms of plantar fasciitis. This condition develops as a result of the plantar fascia becoming torn, which may often be due to excessive strain the foot endures during physical activity. When this band of tissue that runs along the bottom of the foot becomes injured, patients will most likely feel intense heel pain. It’s important to have a proper diagnosis performed, and this may be accomplished by undergoing an MRI in addition to a physical examination. There are many treatment options available, and it’s suggested to schedule a consultation with a podiatrist who can choose the best one for you.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Richard Silverstein from Union Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Why it is Important to Properly Stretch the Feet and Ankles
 Many people who are involved in sporting activities have experienced the pain and discomfort of foot and ankle injuries. It may typically result in significant downtime from running or jumping to allow for proper healing to begin. There are several ways to possibly prevent foot and ankle injuries from occurring, including warming up the muscles before starting to run, properly stretching the muscles in the foot and ankle, in addition to gradually increasing the time spent on the chosen activity. It’s important to wear proper shoes for walking and running, and this may aid in preventing any trauma inflicted on the foot and ankle. Ankle sprains are a very common injury to endure, as well as an Achilles tendon rupture or tear. This type of injury may affect the plantar fascia, which is tissue that is located on the bottom of the foot that connects the heel to the toes. If you are experiencing any pain in the foot or ankle, it’s suggested to speak with a podiatrist as soon as possible.
Many people who are involved in sporting activities have experienced the pain and discomfort of foot and ankle injuries. It may typically result in significant downtime from running or jumping to allow for proper healing to begin. There are several ways to possibly prevent foot and ankle injuries from occurring, including warming up the muscles before starting to run, properly stretching the muscles in the foot and ankle, in addition to gradually increasing the time spent on the chosen activity. It’s important to wear proper shoes for walking and running, and this may aid in preventing any trauma inflicted on the foot and ankle. Ankle sprains are a very common injury to endure, as well as an Achilles tendon rupture or tear. This type of injury may affect the plantar fascia, which is tissue that is located on the bottom of the foot that connects the heel to the toes. If you are experiencing any pain in the foot or ankle, it’s suggested to speak with a podiatrist as soon as possible.
Foot and ankle trauma is common among athletes and the elderly. If you have concerns that you may have experienced trauma to the foot and ankle, consult with Dr. Richard Silverstein from Union Foot Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Foot and ankle trauma cover a range of injuries all over the foot; common injuries include:
- Broken bones
- Muscle strains
- Injuries to the tendons and ligaments
- Stress fractures
Symptoms
Symptoms of foot and ankle injuries vary depending on the injury, but more common ones include:
- Bruising
- Inflammation/ Swelling
- Pain
Diagnosis
To properly diagnose the exact type of injury, podiatrists will conduct a number of different tests. Some of these include sensation and visual tests, X-rays, and MRIs. Medical and family histories will also be taken into account.
Treatment
Once the injury has been diagnosed, the podiatrist can than offer the best treatment options for you. In less severe cases, rest and keeping pressure off the foot may be all that’s necessary. Orthotics, such as a specially made shoes, or immobilization devices, like splints or casts, may be deemed necessary. Finally, if the injury is severe enough, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot and Ankle Fractures
When the foot or ankle experiences trauma, a fracture may occur. Causes of foot and ankle fractures can vary; in some cases, an obvious impact to the foot or a fall can be behind a fracture. Alternatively, fractures can also occur because of increased stress on the bone over time. The location of the fracture can often give your podiatrist information on how the fracture occurred.
Pain, especially when bearing weight, is a telltale sign of a fracture. Limping due to this pain is a further sign of a foot or ankle fracture. Other symptoms include inflammation, bruising, deformity, and tenderness. A deformity may occur due to a shift in bone alignment or a joint dislocation near the fracture. While pain is a significant symptom of breakage, a patient who has nerve damage or who has diabetes may not feel this pain. In this instance, your podiatrist will look for additional signs to determine whether a fracture has occurred.
If you are experiencing severe pain, cannot walk without limping, have an open wound near the suspected break, or have numbness or tingling in the toes, you should see your podiatrist.
How Increased Weight May Affect the Feet
 Recent research has shown that approximately 70 percent of the population in the Bahamas are obese. This typically impacts the general health of the feet as a result of the additional weight the feet must endure. An increased BMI, or body mass index, generally accompanies any weight that is gained. This may produce unwanted foot conditions that may include plantar fasciitis, tendonitis, arthritis and general “wear and tear” of the bones, ligaments, and tendons. Additionally, the structure of the foot may be negatively affected, which may aid in difficulty maintaining an exercise program. While purchasing shoes, it’s important to choose shoes that fit correctly, which may help to diminish a portion of the pain that may be experienced. If you feel you are obese and would like additional information about this condition on how it may affect the feet, please consult with a podiatrist.
Recent research has shown that approximately 70 percent of the population in the Bahamas are obese. This typically impacts the general health of the feet as a result of the additional weight the feet must endure. An increased BMI, or body mass index, generally accompanies any weight that is gained. This may produce unwanted foot conditions that may include plantar fasciitis, tendonitis, arthritis and general “wear and tear” of the bones, ligaments, and tendons. Additionally, the structure of the foot may be negatively affected, which may aid in difficulty maintaining an exercise program. While purchasing shoes, it’s important to choose shoes that fit correctly, which may help to diminish a portion of the pain that may be experienced. If you feel you are obese and would like additional information about this condition on how it may affect the feet, please consult with a podiatrist.
Obesity has become very problematic at this point in time and can have extremely negative effects on the feet. If you’re an obese individual and are concerned about your feet, contact Dr. Richard Silverstein from Union Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
Since your feet are what support your entire weight when standing, any additional weight can result in pain and swelling. Being overweight is one of the main contributors to foot complications.
Problems & Complications
Extra Weight – Even putting on just a few extra pounds could create serious complications for your feet. As your weight increases, your balance and body will shift, creating new stresses on your feet. This uneven weight distribution can cause pain, even while doing the simplest tasks, such as walking.
Diabetes – People who are overweight are at serious risk of developing type-2 diabetes, which has a drastic impact on the health of your feet. As you get older, your diabetes might worsen, which could lead to loss of feeling in your feet, sores, and bruises. You could also become more prone to various infections.
Plantar fasciitis – Pressure and stress that is placed on muscles, joints, and tendons can trigger plantar fasciitis, which is an inflammation of tissue that forms along the bottom of the foot.
If you have any questions please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Obesity and the Feet
Obesity is a common problem in American society. Approximately one third of the U.S. population is obese. Obesity is defined as a body mass index greater than 30. Obesity has the power to affect different aspects of the body, and one of the most common problems it causes is foot pain. There have been many studies that found a connection between an increased BMI and foot problems. A simple activity such as walking up a flight of stairs can increase pressure on the ankle by four to six times.
Being overweight causes the body to compensate for the extra weight by changing the way it moves. Consequently, people who struggle with obesity commonly have arch problems in their feet. Obesity causes the arch to break by stretching the ligaments and tendons that hold the bones in the foot together. When the arch lowers, the foot may eventually fall flat. Collapsed foot arches fail to provide adequate shock absorption which eventually leads to foot pain. Other conditions that may be caused by flat feet are pronation, plantar fasciitis, weak ankles, and shin splints.
Foot problems that are caused by obesity may be treated by wearing proper footwear. Proper shoes will allow your feet to have better circulation around the arch and ankle. Additionally, those with obesity often discover that typical heel pain remedies are not effective for them. They will find that their plantar fascia is easily injured, and it is often inflamed. The best way to treat this problem is to implement lifestyle changes. A few good ways to improve your diet are to reduce calories, fill up on fruits and veggies, and to limit sugars.
Custom foot orthotics can prevent foot problems if you’re carrying excess weight or are trying to lose weight. The purpose of orthotics is to provide shock absorption to decrease the amount of stress on the joints to prevent arthritis.
Symptoms of Toenail Fungus
 A condition that is referred to as onychomycosis is commonly known as a fungal infection of the toenails. It is common among people who have sweaty feet or enjoy spending time swimming. It may occur as a result of the small fungi seeping through tiny cuts in the skin, or possibly lodging between the nail and the nail bed. It may be common to find this type of infection in the toenails because of the warm environment the shoes and socks provide. There are several symptoms associated with this condition, including having a yellow, white or brown appearance, the nail becoming brittle and breaking easily, or the nail becomes uncomfortable. Despite the unsightly appearance, they typically do not pose a health threat unless the patient is diabetic. Research has shown there may be preventative measures that can be taken, including washing and drying the feet, especially between the toes, trimming the nails properly and frequently, and avoiding wearing other people’s shoes. If you feel you have a toenail fungus, it’s suggested to speak with a podiatrist as quickly as possible for a correct diagnosis and to learn about treatment options.
A condition that is referred to as onychomycosis is commonly known as a fungal infection of the toenails. It is common among people who have sweaty feet or enjoy spending time swimming. It may occur as a result of the small fungi seeping through tiny cuts in the skin, or possibly lodging between the nail and the nail bed. It may be common to find this type of infection in the toenails because of the warm environment the shoes and socks provide. There are several symptoms associated with this condition, including having a yellow, white or brown appearance, the nail becoming brittle and breaking easily, or the nail becomes uncomfortable. Despite the unsightly appearance, they typically do not pose a health threat unless the patient is diabetic. Research has shown there may be preventative measures that can be taken, including washing and drying the feet, especially between the toes, trimming the nails properly and frequently, and avoiding wearing other people’s shoes. If you feel you have a toenail fungus, it’s suggested to speak with a podiatrist as quickly as possible for a correct diagnosis and to learn about treatment options.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Dr. Richard Silverstein of Union Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Possible Treatments of a Broken Ankle
 Research has shown the ankle is comprised of three bones that interlock together. If an injury is endured that fractures one or more of these bones, it is often referred to as a broken ankle. There are several ligaments and tendons that are attached to these specific bones and may become displaced if the ankle becomes fractured. This typically may occur if a fall has happened and the ankle twists unnaturally. The noticeable symptoms may often include severe pain in and around the affected ankle, unsightly bruising, or difficulty in moving the toes. There are several ways to treat this condition, including wearing a protective boot, taping or wrapping the ankle, which may provide additional support, or possible surgery, which is often determined by the severity of the fracture. If you have broken your ankle, it’s advised to speak with a podiatrist as quickly as possible so the correct choice of treatment can begin.
Research has shown the ankle is comprised of three bones that interlock together. If an injury is endured that fractures one or more of these bones, it is often referred to as a broken ankle. There are several ligaments and tendons that are attached to these specific bones and may become displaced if the ankle becomes fractured. This typically may occur if a fall has happened and the ankle twists unnaturally. The noticeable symptoms may often include severe pain in and around the affected ankle, unsightly bruising, or difficulty in moving the toes. There are several ways to treat this condition, including wearing a protective boot, taping or wrapping the ankle, which may provide additional support, or possible surgery, which is often determined by the severity of the fracture. If you have broken your ankle, it’s advised to speak with a podiatrist as quickly as possible so the correct choice of treatment can begin.
Broken ankles need immediate treatment. If you are seeking treatment, contact Dr. Richard Silverstein from Union Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our office located in Havre de Grace, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
All About Broken Ankle
Broken ankles or “ankle fractures” are injuries that occur when the bones that make up the ankle joint are broken. Ankle injuries are some of the most common bone and joint injuries. The ankle joint is made up of three bones that join. The tibia is the main bone, and it makes up the inside of the anklebone. The fibula is a smaller bone, and it makes up the outside of the anklebone. A membrane called the joint capsule is lined with a layer called the synovium, which covers the entire joint. The synovium produces synovial fluid which allows for the joint surfaces to move.
An ankle becomes broken when the joint is stressed beyond the strength of its limits. When an ankle is fractured, ligaments may also tear at the same time. Fractures often occur to the ankle rolling or twisting in an unusual way. At times, a fracture may even be caused by an extreme force applied to the joint.
Symptoms of a broken ankle include pain, swelling, bruising, discoloration, numbness, and an inability to move the toes. If you have a broken ankle, you may also hear something tear or snap when you initially suffered the injury. If you have pain from a broken ankle, beware that the pain will not always come from the exact area of the fracture; you may also experience pain from associated foot fractures. The swelling you may experience can suggest that soft tissue damage may have occurred due to the injury.
There are differences between an ankle fracture and an ankle sprain. The difference is that a fracture or break in the bone is required to classify an injury as a broken ankle. An ankle sprain occurs when there is a tear or disruption of ligaments in the ankle. In some cases, the prognosis of an ankle sprain may be worse than that of a fracture.
X-rays are the most common way to diagnose a broken ankle. X-rays show if the ankle is broken and where exactly the fracture is located. It will also show how many pieces of broken bone there are. A second method of testing to see if an ankle is broken is a stress test. To do this, the doctor will put pressure on the ankle and perform a stress test to determine if the fracture requires surgery. Other methods for diagnosis include CT scans and MRI scans.
If you are suffering from a broken ankle, consult with your podiatrist immediately to receive a proper diagnosis and treatment.